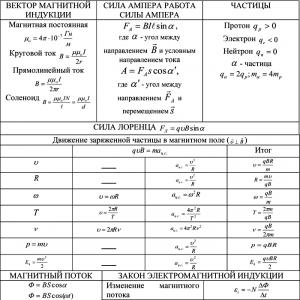
What is the direction of the electric current along the lead axis. Vector image of electrical quantities (current, voltage, emf)
Vector image of electrical quantities (current, voltage, emf). Note on complex numbers for calculating electrical circuits. Representation of sinusoidal emfs, voltages and currents by complex numbers
When depicting rotating vectors of sinusoidal emf, voltage and current on the complex plane, the abscissa axis of the Cartesian coordinate plane is aligned with the axis of real or real quantities (axis + 1) of the complex plane. Then the instantaneous values of sinusoidal quantities are obtained on the axis of imaginary quantities (axis+j).
As is known, each vector on the complex plane corresponds to a certain complex number, which can be written in exponential, trigonometric or algebraic form. For example, e.m.f. Emsm (cot + c/s) shown in Figure 9.1 as a rotating vector corresponds to a complex number.
Figure 9.1 - Image of a sinusoidal emf. rotating vector on the complex plane
Um=Um+jUm, (9.1)
Em ef(ут+ше)= Em cos(уt+шe)+jEmsi n+(ут+шe)= e"+je (9.2)
Phase coal a>t+ y/, determined by vector projections on the coordinate axes +1
tg (ут+ше)= e/e" (9.3)
The imaginary component of the complex number of a vector on the complex plane determines the sinusoidal change in emf. and is denoted by the symbol Im
e=Em sin(ут+ше)=Im Em e"(ут+ше). (9.4)
It is convenient to represent the complex number E j(ут+ше) as the product of two complex numbers
Em е"(шт+ше)= Em е" ме e ьt = Em е(шt (9.5)
The first complex number Em corresponding to the position of the vector at the initial moment of time is called the complex amplitude
Em = Em etshe (9.6)
The second complex number Esh is the operator of rotation of the vector by an angle cat relative to the initial position of the vector.
Consequently, the instantaneous value of the sinusoidal quantity is equal to the unsigned imaginary part j of the product of the amplitude complex Em and the rotation operator
e=Em sin(шт+ше)=Im Em еjшt. (9.7)
The transition from one form of recording sinusoidal emf, currents and voltages to another is carried out very simply using the formula
Euler ejsht - cos +/sin a.
If, for example, the complex voltage amplitude is given as a complex number in algebraic form
Um =Um+ jUm (9.8)
then to write it in exponential form, it is necessary to find the initial phase<р „, т.е. угол, который образует вектор Um с осью + 1.
In this case, the vector Um is located in the first quadrant of the complex plane, and its initial phase (Figure 9.2) is determined by the relation
Tg shu=Um /Um (9.9)
Instantaneous voltage values
u=ImUm e ьt =ImUme"(Ут+ше)= Um sin(Ут+ше), (9.10)
Let's consider another example, when the complex amplitude of the current is given by a complex number
Im=-Im+jIm (9.11)
The complex current amplitude vector /m is located in the second quadrant of the complex plane (Figure 9.3). The initial phase of this current
Sht=180є-b (9.12)
Where tgшt=tg(180є-b)=- Im/ Im=tgb (9.13)
If the instantaneous value of the current is given in the form of a sinusoid / = Imsin(o)e + , then the complex amplitude is written first in exponential form, and then, using Euler’s formula, we proceed to the algebraic form

Figure 9.2 - the initial vector of the complex voltage amplitude located in the first quadrant of the complex plane.

Figure 9.3 - the first initial phase of the complex current amplitude vector located in the second quadrant of the complex plane
The use of complex numbers allows us to move from geometric addition or subtraction of vectors on a vector diagram to algebraic action on the complex numbers of these vectors. For example, to determine the complex amplitude of the resulting current (see Figure 9.4), it is enough to add two complex numbers corresponding to the complex amplitudes of the branch currents
I3m= Im +I2m =I3mefш3 (9.16)
To determine the complex amplitude of the resulting emf. (see Figure 9.4) it is enough to determine the difference of the complex numbers corresponding to the complex amplitudes of the emf. Et and Et..
Representing sinusoidal quantities using vectors
When calculating AC circuits, it is often necessary to perform addition and subtraction operations of currents and voltages. When currents and voltages are specified analytically or by timing diagrams, these operations turn out to be very cumbersome. There is a method for constructing vector diagrams that can significantly simplify operations on sinusoidal quantities. Let us show that a sinusoidal quantity can be represented by a rotating vector.
Let the vector 1m rotate with a constant angular frequency c counterclockwise. The initial position of the vector /m is specified by the angle y/ (Figure 9.4.). The projection of the vector 1m onto the y-axis is determined by the expression /„, sin (cot + q/), which corresponds to
instantaneous value of alternating current. Thus, the timing diagram of alternating current is a time sweep of the vertical projection of the vector /t, rotating at speed co.
The representation of sinusoidal quantities using vectors makes it possible to clearly show the initial phases of these quantities and the phase shift between them.

Figure 9.4 - Image of sinusoidal current by rotating vectors
In vector diagrams, the lengths of the vectors correspond to the effective values of current, voltage and emf, since they are proportional to the amplitudes of these quantities.
Figure 9.5 shows vectors Ei and E2 with initial phases c/i and c/2 phase shift

Figure 9.5 - Vector diagram of sinusoidal E.M.F.
A set of several vectors corresponding to the zero point in time is called a vector diagram. It must be borne in mind that in a vector diagram, vectors represent currents (voltages) of the same frequency.

To understand how an electrocardiograph works, what processes in the body it records, and what an electrocardiogram shows, it is necessary to describe the essence of the physical processes that occur during contraction of the heart muscle.
Let's recall elementary knowledge from the school physics and algebra course.
The work of the heart muscle is an electrical process that constantly flows in the body. The space in which the action of electric forces is observed is called electric field. An electric field implies the existence of two charges - positive and negative. Such a tandem of charges is called electric dipole. The figure shows the electric field of a dipole using lines of force. Between the negative and positive charge there is a zero line, at which the magnitude of the charge is zero. At point A, located at a distance R from the center of the dipole (the distance R is much greater than the distance between the charges), the field E (directed tangentially to the field line) is decomposed into two components: E1 - parallel to the dipole axis and E2 - perpendicular to it.
An electric dipole creates potential difference. In general, in order for current to begin to flow in any electrical circuit, some external force of a non-electrostatic nature is necessary. For example, the electric current that we extract from an electrical outlet in everyday life is, by nature, the energy of falling water at a hydroelectric power station, or the energy of a fissionable atom at a nuclear power plant, or the thermal energy of coal at a thermal power plant. The electric current produced in a car is the energy of chemical transformations in the battery, or the energy of burned gasoline in the engine. The electric current that makes our heart work is obtained as a result of biochemical processes constantly flowing in the body. This was very accurately noted in one of the songs of the once popular rock group “Cruise”: “That our life is the metabolism of nature.”
But, let's return to our "rams". The quantity characterizing the source of energy of a non-electrostatic nature in an electrical circuit, necessary to maintain an electric current in it, is called electromotive force(EMF). The emf vector of a dipole is represented by a straight line connecting both of its poles and is directed from the negative to the positive charge.
Let's return to our dipole. EMF is a vector quantity, because characterized by magnitude and direction in space. The EMF is shown as a straight line with an arrow at the end. The length of this straight line characterizes the magnitude of the EMF, and the location in space characterizes the direction.
The zero isopotential line (isopotential means connecting points with the same potential) divides the dipole field into two halves - a positive and a negative field. Isopotential lines located in a positive field are called positive; in a negative field - negative. In the figure, isopotential lines are depicted as concentric ellipses located around positive and negative charges. The largest negative charge is located near the zero line on the side of the negative field, the largest positive charge is located on the side of the positive field. The strength of the charge decreases in inverse proportion to the square of the distance from it.
The founder of electrocardiography, William Einthoven, considered the heart as a source of electric current (during its excitation, an electric field is formed in the body), located in the center of a triangle bounded by the right and left arms, and the left leg ( Einthoven triangle). He made the assumption that the human body is a conductor of current with constant electrical resistance in all areas. The left, right hand, and left leg were taken by him to be three points equidistant from each other and from the center (where the heart is located), lying in the same frontal plane. Einthoven suggested that, arising during the excitation of the heart, the EMF vector also shifted only in the frontal plane. Subsequently, this theory was supplemented and revised, because different parts of the human body have different resistance, and the electric field of the heart constantly changes in magnitude and direction and changes not only in the frontal projection. Numerous further studies have confirmed the applicability of the dipole theory in clinical electrocardiography.
To measure the potential value at various points in the field, use galvanometers- the main unit of the electrocardiograph. EMF is measured using two electrodes, which are connected to the positive and negative poles of the galvanometer.
A galvanometer has two types of electrodes: an active (different) electrode and an inactive (indifferent) electrode. The inactive electrode has a charge close to zero (we can say that this is an electrical “mass”, by analogy with a car battery) and is connected to the negative pole of the galvanometer. The active electrode is connected to the positive pole of the galvanometer and indicates the potential of the point in the electric field at which it is located. If the active electrode is in the region of a positive field, then the galvanometer records the rise of the curve from the isoline (positive tooth); if in the area of a negative field, a decrease in the curve (negative wave) is recorded.
You should know that a galvanometer registers potential differences. That is, the device will record a change in the curve if a charge of the same sign, but different in magnitude, is applied to both electrodes.
ATTENTION! Information provided on the site website is for reference only. The site administration is not responsible for possible negative consequences if you take any medications or procedures without a doctor’s prescription!
Indications for emergency electrical cardiac defibrillation (EDC):
In all cases of VF (with large or small amplitude, tonic or atonic) - urgently, without wasting time on intubation and cardiac massage, EDS can restore sinus rhythm, which will eliminate the need for external cardiac massage;
VT with a clinical picture of circulatory arrest (no pulse in the carotid artery, the patient is unconscious);
“blind” EDS (i.e. defibrillation in the absence of ECG diagnostics) is rarely necessary, since most universal defibrillators are equipped with an ECT monitor. There is no evidence of the usefulness of EDS in asystole. Sometimes small-wave VF occurs in the form of asystole. In such cases, re-diagnosis of the type of cardiac arrest is necessary;
Rice. 33.1. Electrodefibrillation
EMF in synchronization mode (synchronized cardioversion) is recommended for the relief of paroxysmal supraventricular tachycardia, atrial fibrillation and flutter. Synchronization of supplied energy reduces the possibility of induction FJ, which can happen if the discharge occurs during the relative refractory phase.
The basic principle of EMF is that under the influence of a powerful and short-range (0.01 s) electrical impulse, depolarization of all myocardial muscle fibers occurs with the subsequent development of refraction, after which the impulse from the sinus node is able to restore spontaneous heart contractions.
Device of electric defibrillators. Electric defibrillators can be of two types - alternating current and direct current.
Currently, discharge-type rechargeable defibrillators are most widely used. Their weight is from 8 to 10 kg, they are compact, simple and easy to use, equipped with a monitor screen that allows you to receive an instant signal from paddle-shaped electrodes, which are also electrodes for recording ECG with subsequent printing of data on a plotter or built-in matrix printer . Defibrillators of this type are indispensable when working in severe emergency conditions, and in an ambulance during transportation of a victim, etc. One of the best defibrillators is FC-200 (Japan).
The basis of successful EDS depends to a certain extent on the training and knowledge of medical personnel. If the device is well studied, then technical delays in preparing the defibrillator for operation can be avoided. Let us briefly look at some noteworthy technical characteristics of the operation of discharge-type rechargeable defibrillators.
Operating principle of an electric defibrillator (ED) consists of the formation of energy as a result of the discharge of a capacitor pre-charged to a certain voltage. In this case, a single current pulse is generated, which has the form of a damped oscillatory discharge.
Various ED designs differ from each other in capacitor capacity (from 16 to 20 μF) and give a correspondingly different shape to the current pulse. The strength of electrical impulses is determined using the units of energy received and used during discharge. This energy is determined in joules (watt / s).
When starting to study the defibrillator, pay attention to the pulse energy range indicated on the front panel. On the domestic defibrillator DKI-N-04, pulses with energies of 5, 10, 25, 50, 75 J are used for direct defibrillation, and for indirect defibrillation - 100, 150, 200, 250, 300, 350 J, while while one of the imported versions of the ED (MS-730) uses 5, 10, 25, 60 and 100, 200, 360 J, respectively. It is possible to designate energy in the form of numbers “I, 2, 3, 4”, the interpretation of which is given in the table on the ED housing.
The electrodes can be different in technical design and marking. For EDS in adults, both hand electrodes or one padded electrode must have a platform with a diameter of 8-14 cm. In the latest EDS samples, they are marked with the designations “Apex” and “Sternum”, allowing you to quickly and accurately place the electrodes on the desired areas of the chest. The defibrillator electrodes are aligned with the ECG electrodes. Other markings of ED electrodes are also possible, for example black (carrying a negative charge) and red (carrying a positive charge). Sometimes the electrodes are equipped with a spring device, which allows achieving optimal pressing force of the electrodes to the chest (10-15 kg). If there is no such pressing force, then the defibrillator will not work. A prerequisite for EMF is to lubricate the electrodes with a special electrode paste or place gauze pads moistened with an isotonic sodium chloride solution under them to reduce the resistance of the chest when current passes. In order to optimally distribute the current, the electrode plates during external defibrillation should have a diameter of 12-14 cm for adults, 8 cm for children and 4.5 cm for infants. For direct defibrillation, the electrode size should be 6 cm in diameter for adults, 4 cm for children and 2 cm for infants.
Methods of electrical defibrillation of the heart. There are electrical defibrillation of the heart: indirect (external), when the defibrillator electrodes are applied to the chest, and direct, when the electrodes are applied directly to the heart with the chest open.
When performing external defibrillation, two options for the location of electrodes are possible: 1) anterior, or standard, location, when one electrode marked “Apex”, or red (positive charge), is placed exactly above the apex of the heart or below the left nipple; another electrode marked “Sternum”, or black (negative charge), is placed immediately under the right clavicle (see Fig. 33.1), 2) anteroposterior location of the electrodes - one electrode plate is located in the right subscapular region, the other - anteriorly above the left atrium. Safety is achieved by good isolation of the electrodes using paste or gel between the electrode pad and the chest so that the electric current does not pass through the chest, bypassing the myocardium.
If cardioversion or defibrillation is performed in a patient with a permanent pacemaker, it is necessary to avoid close proximity of the electrodes and the pacemaker to avoid damage to the latter. After the EMF, the pacemaker should be checked.
EMF depends on the chosen energy level to generate adequate transmyocardial potential. If the energy and current levels are too low, the EMF will not stop the arrhythmia, but if they are too high, functional and morphological disturbances may occur. Defibrillation is carried out by passing a current (measured in A) through the heart. The current strength is determined by the discharge energy (J) and transthoracic impedance (Ohm). There is no exact relationship between body size and the level of energy required for defibrillation in adults. In this case, transthoracic impedance plays a decisive role. Factors determining the latter include the selected energy, the size of the electrodes, the number and time of previous shocks, the phase of ventilation, the distance between the electrodes and the pressure exerted on the electrode. A significant increase in transthoracic impedance occurs when using electrodes that are not lubricated with electrode paste and with low pressure on the electrode. On average, in an adult, the transthoracic impedance is 70-80 ohms.
Select energy level and current. The AKA recommended energy level for the first shock should be 200 J, for the second shock - from 200 to 300 J. The establishment of a range of energy levels is due to the fact that any of the specified levels can lead to successful defibrillation. If the first two defibrillation attempts are unsuccessful, a third shock of 360 J should be given immediately. If VF is interrupted after the shock and then resumes, defibrillation should be given at the same energy level. The shock is increased only if defibrillation attempts are unsuccessful. If three shocks are unsuccessful, continue CPR, administer adrenaline, and then repeat the shocks. In out-of-hospital settings, defibrillation should be performed immediately upon delivery of the defibrillator.
According to AKA recommendations, the energy for cardioversion in VT with or without pulse deficit is 100 J. For polymorphic ventricular tachyarrhythmias, cardioversion is carried out according to the same scheme as for VF.
In addition to the correct choice of energy, the correct choice of current strength is necessary. Low energy levels and high transthoracic impedance result in too little current and ineffective defibrillation. Too high an energy level with a low transthoracic impedance causes the use of a higher shock intensity, which leads to myocardial damage and defibrillation failure. Clinical studies have shown that during defibrillation or cardioversion, the optimal current strength is 30-40 A.
Recently, automatic and semi-automatic defibrillators have been used, which have undoubted advantages compared to known types of defibrillators. Defibrillation using automatic or semi-automatic defibrillators can be performed quickly even by relatively untrained personnel.
PRECORDIAL STROKE
If a patient under cardiac monitoring develops VF, then the immediate goal of treatment should be to restore an effective heart rhythm. In the absence of a defibrillator prepared for use, the doctor, without wasting time, should use a technique called precordial shock. A precordial stroke is an attempt at a reflex effect on the myocardium by converting mechanical energy into electrical potential, restoring the normal rhythm of the heart. Its implementation is mandatory in the presence of cardiomonitoring. The second condition is changes in ECT, which serve as an indication for this type of preliminary therapy.
Indications for a precordial beat:
FJ. An immediate hard blow to the heart after established VF can sometimes be effective. It only takes seconds for a precordial shock to occur while the defibrillator is being prepared. In case of its inefficiency, an EMF should be immediately produced;
VT leading to cardiac VF. According to various authors, the effectiveness of the precordial stroke in VT ranges from 11 to 25%; in VF, restoration of the normal rhythm occurs much less frequently.
In other cases, the Precordial Strike is ineffective. The resuscitator decides on the indications for precordial stroke independently, the approach is individual.
Technique of precordial strike. A punch to the center of the sternum in the precordial area is applied from a distance of at least 30 cm. The blow should be powerful, but not extremely strong (Fig. 33.2). Since precordial shock is only occasionally effective in interrupting VF, it should not be used in place of electrical defibrillation. It is usually indicated for the relief of prehospital VF. This technique is not included in the SL R program for persons without medical education. The precordial beat can convert VT to asystole and VF or to EMD.
EMERGENCY ELECTRICAL HEART STIMULATION
Electrical cardiac stimulation (ECS) is often the only possible treatment option in emergency situations. Indications for ESS are various rhythm disturbances, accompanied by hemodynamic disorders and not eliminated by drug therapy.
Emergency ESA is indicated in all cases of severe bradycardia accompanied by inadequate circulation (systolic blood pressure less than 80 mm Hg), impaired consciousness, myocardial ischemia or pulmonary edema. Emergency ESA is also performed for complete heart block, symptomatic second degree heart block, sick sinus syndrome, bradycardia caused by drugs (digoxin, β-blockers, calcium channel blockers, procainamide), idioventricular bradycardia, symptomatic atrial fibrillation with a slow ventricular rhythm, refractory bradycardia that occurs during hypovolmic shock, bradyarrhythmia with malignant changes in the ventricular rhythm. Atropine, usually used for bradycardia, should be prescribed with caution in patients with acute myocardial infarction, since it increases heart rate and may increase myocardial ischemia.

Rice. 33.2. Precordial beat.
The indication for emergency ESA is bralycardia with periods of asystole, tolerant to pharmacotherapy. Sometimes bradycardia alternates with periods of VT. Increasing heart rate using ESA can lead to the disappearance of such rhythms, while antiarrhythmic drugs are ineffective in these cases.
In case of bradysystole, ESA is not recommended as the main method of CPR. If complex CPR does not give a positive result, ESA should be used as soon as possible. Typically, ESS is ineffective for asystole and EMD due to deep myocardial ischemia. ESA is indicated for malignant forms of atrial and ventricular tachycardia that are not eliminated by drug therapy and cardioversion. In these cases, the Overcliive mode is used: stimulation in the Chechen for several seconds at a higher frequency than the heart rate of Syulyugo. Then stimulation is stopped with the expectation that the normal rhythm will be restored). This technique is possible for supraventricular and ventricular tachycardias. It turns out to be very useful in unstable conditions.
Temporary ESA is performed for severe bradycardia that is not accompanied by severe hemodynamic disturbances.
For patients who are currently clinically stable, but have a high probability of decompensation in the near future (stable bradycardia without hemodynamic disturbances, symptomatic sinus node dysfunction, atrioventricular block type Mobitz II, heart block III degree, etc.) , it is recommended to install the pacemaker in stand-by mode. This allows you to prevent unwanted emergency situations. In the intraoperative period, severe forms of bradycardia that are not amenable to drug therapy and are accompanied by a decrease in blood pressure can be stopped using temporary transesophageal ESS.
REVIVAL WITH DIRECT HEART MASSAGE
Direct cardiac massage should not be used as a normal, routine method of CPR, since chest compressions are quite effective. At the same time, in some cases, due to the impossibility of revival using external compression of the sternum, direct cardiac massage is required. In animal experiments, it was shown that direct cardiac massage, performed after a short, ineffective chest compressions, improved the survival of animals. However, in clinical practice, direct cardiac massage is often used at a later date and there is no direct evidence of its benefit. Clinical studies have confirmed that direct massage when used late (25 minutes after cardiac arrest) is ineffective. Therefore, it should not be used as a last attempt at resuscitation after non-invasive CPR has failed.
Main indications for direct cardiac massage:
Cardiac tamponade causing cardiac arrest can in most cases be eliminated by direct emptying of fluid (usually blood) from the pericardial cavity. Cardiac tamponade can occur due to various factors;
With extensive pulmonary thromboembolism, chest compressions are usually ineffective. If the diagnosis of embolism is established or there is at least an assumption of the presence of this complication, the last attempt may be thoracotomy, direct cardiac massage, surgical removal of the embolus;
In deep hypothermia, direct cardiac massage has several advantages. With hypothermia, persistent VF often occurs, which is sometimes not eliminated by repeated defibrillation with the chest closed. During resuscitation, the heart and chest cavity can be flushed with warm isotonic sodium chloride solution. This will ensure greater efficiency of the method;
Penetrating wounds of the chest and abdominal cavity, blunt trauma with a clinical picture of cardiac arrest (immediate thoracotomy + direct cardiac massage);
Deformations of the chest, sternum, spine, and displacement of the mediastinum can interfere with chest compressions. Indirect cardiac massage may also be ineffective due to loss of elasticity of the chest. The fragility of the chest leads to multiple fractures. Carrying out emergency thoracotomy, direct cardiac massage and defibrillation requires the rapid work of a well-coordinated team of specialists, which is possible in an operating room.
In recent years, there has been renewed interest in direct cardiac massage. Data are presented that CO, which during closed cardiac massage is equal to 30% of the proper value, under direct massage conditions is 2.5 times higher than this level. There is also experimental and clinical evidence that coronary and cerebral blood flow during direct cardiac massage reaches 50 and 90% of the initial level, respectively. This evidence has not yet received recognition, but it cannot be ignored.
OTHER METHODS OF CARDIOPULMONARY RESUSCITATION
Extracorporeal membrane oxygenation. This method is used only in clinical settings and most often for hypothermic cardiac arrest. Coordinated work of specialists, quick access to the main vessels, availability of ready-to-fill systems for extracorporeal circulation, etc. are required. The method can be used as an alternative to direct cardiac massage.
Creation of constantly increased abdominal pressure. The essence of the method is to create a constantly increased intra-abdominal pressure by tightly pulling the abdomen or using anti-shock trousers during external cardiac massage.
This method helps to increase arterial and coronary perfusion pressure and increase CO. However, there is not yet sufficient confirmation of the advantages of this method in clinical settings. It should be emphasized the danger of liver injury due to compression of the abdomen.
Intercalated abdominal compression. The method is based on compression of the abdomen in the interval between two successive chest compressions during CPR. Intercalated abdominal compression in the relaxation phase corresponds to CPR diastole. The frequency of compression is 80-100 per 1 min. It is carried out through the coordinated work of two resuscitators.
Experimental studies of the use of the method in the clinic confirm that the addition of CPR with insertional abdominal compressions significantly increases coronary perfusion pressure and improves the survival rate during circulatory arrest in the hospital.
The use of special inflatable vests. The essence of this method is that a special air vest is put on the patient’s chest, periodically inflating which causes artificial systole and artificial exhalation. Diastole and inspiration occur passively. As a result, the perfusion pressure in the aorta and coronary vessels increases and, compared with the standard CPR technique, a slight increase in the rate of restoration of spontaneous circulation and short-term survival of patients is achieved. Research is currently being conducted to further improve this method.
Active compression-decompression. The active compression-decompression method is based on the assumption that blood flow during CPR is associated not so much with compression of the heart itself, but with compression of all vascular capacities of the chest. Alternating compression and decompression of the chest makes not only systole active, but also diastole. This is achieved using a hand-held device - a “car-diopamp”, reminiscent in design of a household plunger. The “cardio pump” is placed on the surface of the chest and periodically creates a vacuum using suction, which results in an increase in CO, coronary perfusion pressure, negative inspiratory pressure, MOB and systolic blood pressure. There is no need for mechanical ventilation with this method. However, an indispensable condition for its adequacy as a component of the method is restored airway patency. Active chest decompression improves venous return to the heart, resulting in an increase in left ventricular volume and stroke volume, as well as CO and BP. Blood pressure becomes higher than with standard CPR.
Despite the development of new approaches to resuscitation, the main CPR technique remains indirect cardiac massage. Further improvements and convincing clinical evidence of the benefits of new resuscitation techniques are required.
Chapter 34
CARDIOPULMONARY RESUSCITATION TRAINING PROGRAM
Statistics show that more than 20% of lives could be saved if the person at the scene of the accident knew first aid and CPR. There are currently 50 million people abroad trained in CPR techniques. How many people are trained in these techniques in Russia? We do not have such data, but we believe that, at best, 10-20 thousand people. Training in the basics of CPR is carried out in the Russian Federation at the departments of medical institutes, in large scientific centers, the Institute of General Resuscitation of the Academy of Medical Sciences and in certain regions (Irkutsk). The difficulties with organizing such training in the Russian Federation lie primarily in the lack of funds necessary to organize CPR courses. Therefore, training in certain regions is carried out at the expense of organizations that are interested in this. There are almost no technical training aids (simulators, mannequins, audio-video equipment). Mannequins purchased abroad are very expensive. We believe that the organization of permanent courses in first aid and CPR should be introduced into the rank of state policy, i.e. priority measures aimed at reducing the consequences of injuries, various accidents and environmental disasters in our country. Many, without receiving timely help, become disabled for the rest of their lives. Even if the injury is not severe, its impact on health, social and economic problems is enormous.
Indeed, it is possible to save people in cardiac arrest or loss of consciousness in a public place or far out in the country if someone quickly administers life-sustaining first aid and then calls an ambulance. Many lives could have been saved if the first person to help had learned CPR techniques. Basic life support means not only maintaining signs of life, but also gaining time until the ambulance arrives. To effectively spread the skill of CPR in society, it is necessary to have a training program on a large scale. The CPR training program should include two aspects: 1) training for persons without medical education; 2) training of students of medical institutes and schools, doctors and all medical personnel. In this version of the program, materials from other well-known programs (Laerdal company, etc.) are used.
CASCADE PRINCIPLE OF TRAINING
The cascade principle of CPR training provides for two levels of instructors: instructor-teacher and simple instructor. The instructor-teacher is a well-trained doctor who is fluent in CPR techniques. Just an instructor - it can be a person with a medical (doctor, paramedic, nurse) or without a medical education, but who has undergone special training (“paramedic”). The instructor-teacher must train new instructor-teachers and the instructors themselves, while the instructor only trains rescuers. The cascading principle is that one instructor-teacher can train 6 new instructor-teachers in one course. After the first course, everyone will be able to train 36 instructors. During the year, each of the 36 will be able to conduct 6 courses and train up to 1296 rescuers in 1 year.
A high assessment of the cascade principle of learning is that there is a rapid increase in the number of trainees with a minimum expenditure of time. Each instructor works less than 20 hours a year. It is important that the programs are standard and can be used for a long time.
The goal of the program is to teach CPR techniques to a large number of people. There is an additional program for people with medical education and students. It is necessary to widely promote the CPR program among the organized population (schools, the Ministry of Internal Affairs, enterprises).
Preparation for the CPR course. Ideally, there should be a specially equipped training room. For training you need:
video, tables, posters;
guide CPR;
self-study guide (Laerdahl);
a complete set of first aid equipment;
training mannequin (dummy) - 1 for 2 cadets;
mask for ventilation;
maps (explaining the stages of first aid), slides;
certificates completed and signed by the instructor.
Course structure. Each instructor (as well as a teacher at a medical university) should not have more than 6 students in the course. The course lasts 4 hours.
Introduction (5 min). The instructor must introduce himself and familiarize the cadets with the purpose of training. It is desirable to assess the general level of knowledge of the cadets;
Video presentation on the basics of CPR (20 min). The rest of the time is allocated for practical mastery of the material;
The instructor demonstrates each stage of CPR and then each student repeats these techniques. The instructor controls every element of the practical training; the final result depends on the correct execution of the techniques;
Pointing out errors. In case of failure to master the material, additional classes are prescribed;
Assessment of theoretical and practical knowledge. Theoretical knowledge is assessed in writing. Practical skills are tested on mannequins and dummies. To do this, a cadet or group of cadets are given tasks (for example, a car accident has occurred, the driver has cardiac arrest, one passenger has signs of asphyxia, another has lost consciousness. Quickly navigate the situation and provide appropriate assistance). Great importance is attached to the diagnosis of disorders of vital functions: consciousness, breathing and circulation. Each cadet must complete all elements of practical training; 4 cycles of CPR. A certificate (certificate) is received by cadets who complete the course;
Intensive therapy and anesthesia support for...
BASIC PROFESSIONAL EDUCATIONAL PROGRAM OF POST-GRADUATE PROFESSIONAL EDUCATION IN SPECIALTY No.
Management2000 “Cardiopulmonary resuscitation. Pocket Guide" Groer K., Cavallaro D., 1996 " Intensivetherapy. Reanimation. Firsthelp" Malyshev V.D. , Educational...
What is electrocardiography?
Electrocardiography is a method of graphically recording electrical phenomena occurring in the beating heart. The spread of excitation throughout the heart is accompanied by the appearance of an electric field in the volumetric conductor (body) surrounding it. The shape, amplitude and sign of the elements of the electrocardiogram depend on the spatiotemporal characteristics of the excitation of the heart (chronotopography of excitation), on the geometric characteristics and passive electrical properties of the body as a volumetric conductor, on the properties of the electrocardiogram leads as a measuring system.Each muscle fiber is an elementary system - a dipole.
From countless microdipoles of single myocardial fibers, a total dipole (EMF) is formed, which, when the excitation propagates in the head part, has a positive charge, and in the tail part - a negative one.
With the extinction of excitation, these ratios become opposite. Since excitation begins at the base of the heart, this region is the negative pole, the apex region is the positive pole.
The electromotive force (EMF) has a certain magnitude and direction, i.e. is a vector quantity. The direction of the EMF is usually called the electrical axis of the heart; most often it is located parallel to the anatomical axis of the heart. A line of zero potential runs perpendicular to the electric axis.
With the help of electrocardiographs, the biocurrents of the heart can be recorded in the form of a curve - an electrocardiogram (ECG).
The development of electrocardiography is associated with the name of the Dutch scientist Einthoven, who first recorded the biocurrents of the heart in 1903.
using a string galvanometer and developed a number of theoretical and practical foundations of electrocardiography.
The main functions of the heart:
The heart has a number of functions that determine the characteristics of its work:1) the function of automatism. It is the ability of the heart to produce electrical impulses in the absence of any external stimulation.
The cells of the sinoatrial node (SA node) and the conduction system of the heart have the function of automaticity: the atrioventricular junction (AV junction), the conduction system of the atria and ventricles. They are called pacemaker cells.
The contractile myocardium lacks an automatic function.
The SA node is the center of first-order automaticity. Normally, this is the only pacemaker that suppresses the automatic activity of the other (ectopic) pacemakers of the heart.
The function of the SA node and other pacemakers is greatly influenced by the sympathetic and parasympathetic nervous systems: activation of the sympathetic system leads to an increase in the automaticity of the cells of the SA node and conduction system, and the activation of the parasympathetic system leads to a decrease.
The SA node produces electrical impulses at a frequency of 60-80 per minute.
Centers of second-order automaticity - some areas in the atria and the AV connection - the zone of transition of the atrioventricular node into the His bundle. The frequency of produced electrical impulses is 40-60 per minute.
Third-order centers of automaticity, which have the lowest ability for automaticity (25-45 impulses per minute), are the lower part of the His bundle, its branches and Purkinje fibers. Automatic centers of the second and third order are only potential, or latent, pacemakers; they take on the function of a pacemaker in case of lesions of the SA node;
2) conductivity function. This is the ability to conduct excitation arising in any part of the heart to other parts of the heart muscle. The wave of excitation generated in the cells of the SA node propagates along the intraatrial pathways - from top to bottom and slightly to the left, at the beginning the right atrium is excited, then the right and left atrium, and at the end - only the left atrium.
In the AV node there is a physiological delay in the excitation wave, which determines the normal time sequence of excitation of the atrium and ventricles.
From the AV node, the excitation wave is transmitted to a well-developed intraventricular conduction system, consisting of the atrioventricular bundle (bundle of His), the main branches (legs) of the bundle of His and Purkinje fibers;
3) excitability function and refractoriness of myocardial fibers.
Excitability is the ability of the heart to become excited under the influence of impulses. The cells of both the conduction system and the contractile myocardium have an excitability function.
The occurrence of excitation in the muscle fiber is the result of changes in the physicochemical properties of the cell membrane and the ionic composition of the intracellular and extracellular fluid. During the refractory period, myocardial cells are not excitable to an electrical stimulus (systole). During diastole, the excitability of the myocardial fiber is completely restored, and its refractoriness is absent;
4) contractility function.
Contractility is the ability of the heart muscle to contract in response to stimulation. This function is mainly possessed by the contractile myocardium. As a result of the sequential contraction of various parts of the heart, the main, pumping, function of the heart is carried out.
Operating principle of the electrocardiograph:
Fluctuations in the potential difference that occur when the heart muscle is excited are perceived by electrodes located on the body of the subject and fed to the input of the electrocardiograph. This extremely low voltage passes through a system of cathode lamps, due to which its value increases by 600-700 times. Since the magnitude and direction of the EMF changes all the time during the cardiac cycle, the galvanometer needle reflects voltage fluctuations, and its fluctuations in turn are recorded as a curve on a moving tape.The galvanometer oscillations are recorded on a moving tape immediately at the time of recording. The movement of the tape for recording ECG can occur at different speeds (from 25 to 100 mm/s), but most often it is 50 mm/s. Knowing the speed of the tape, you can calculate the duration of the ECG elements.
So, if the ECG is recorded at a normal speed of 50 mm/s, 1 mm of the waveform will correspond to 0.02 s.
For ease of calculation, in devices with direct recording, the ECG is recorded on paper with millimeter divisions. The sensitivity of the galvanometer is selected in such a way that a voltage of 1 mV causes a deviation of the recording device by 1 cm. The sensitivity or degree of amplification of the device is checked before recording the ECG; it is carried out using a standard voltage of 1 mV (control millivolt), the supply of which to the galvanometer should cause deviation of the beam or pen by 1 cm. The normal millivolt curve resembles the letter “P”, the height of its vertical lines is 1 cm.
Electrocardiographic leads:
Changes in the potential difference on the body surface that occur during heart activity are recorded using various ECG lead systems. Each lead records the potential difference that exists between two different points in the heart's electrical field where the electrodes are installed.Thus, various ECG leads differ from each other primarily in the areas of the body from which the potentials are removed.
Currently, 12 ECG leads are most widely used in clinical practice, the recording of which is mandatory for each electrocardiographic examination of a patient: 3 standard leads, 3 enhanced unipolar limb leads and 6 chest leads.
Standard leads:
Standard bipolar leads, proposed in 1913 by Einthoven, record the potential difference between two points of the electric field, remote from the heart and located in the frontal plane of the body, on the limbs.To record these leads, electrodes are placed on the right arm (red marking), left arm (yellow marking) and left leg (green marking). These electrodes are connected in pairs to an electrocardiograph to record each of the three standard leads. The fourth electrode is installed on the right leg to connect the ground wire (black marking). Standard limb leads are recorded the next time the electrodes are connected in pairs.
Lead I - right hand (–) and left hand (+).
Lead II - right arm (–) and left leg (+).
Lead III - left leg (+) and left arm (–).
Three standard leads form an equilateral triangle (Einthoven's triangle), the vertices of which are the right arm, left arm and left leg with electrodes installed there. In the center of the triangle is the electrical center of the heart, equally distant from all three leads.
The hypothetical line connecting the two electrodes involved in the formation of the ECG lead is called the lead axis.
If the EMF of the heart at any point in the cardiac cycle is projected onto the positive part of the lead axis, a positive deviation (positive R, T, P waves) is recorded on the ECG. If the EMF of the heart is projected onto the negative part of the lead axis, negative deviations are recorded on the ECG (Q, S waves, sometimes negative T or P waves).
To facilitate the analysis of ECG readings recorded in standard leads, it is customary to slightly shift the axes of these leads and conduct them through the electrical center of the heart. This results in a triaxial coordinate system convenient for analysis.
Reinforced unipolar limb leads. These leads were proposed by Goldberger in 1942.
AVR - enhanced unipolar right arm abduction.
AVL - enhanced unipolar lead from the left arm.
AVF - enhanced unipolar abduction from the left leg.
Six-axis coordinate system:
Standard and enhanced unipolar limb leads make it possible to record changes in cardiac EMF in the frontal plane, i.e. in the plane in which the Einthoven triangle is located.The six-axis coordinate system (Bailey) is obtained by combining the axes of three standard and three enhanced limb leads drawn through the electrical center of the heart. Thanks to it, it is possible to quite accurately determine the magnitude and direction of the EMF vector of the heart in the frontal plane.
Chest leads:
In order to more accurately diagnose myocardial lesions, an ECG is recorded when the electrode is placed on the anterior surface of the chest.Lead V1 - the active electrode is installed in the IV intercostal space along the right edge of the sternum.
Lead V2 - the active electrode is located in the IV intercostal space along the left edge of the sternum.
Lead V3 - the active electrode is located between the second and fourth positions, approximately at the level of the IV rib along the left parasternal line.
Lead V4 - the active electrode is installed in the V intercostal space along the left midclavicular line.
Lead V5 - the active electrode is located at the same horizontal level as V4, on the left anterior axillary line.
Lead V6 - the active electrode is located on the left mid-axillary line at the same horizontal level as the electrodes of leads V4 and V5.
Unlike standard and enhanced limb leads, chest leads record changes in cardiac EMF predominantly in the horizontal plane.
Electrocardiographic deviations in each of the 12 leads reflect the total EMF of the entire heart, i.e. are the result of the simultaneous influence on this lead of a changing electrical potential in the left and right parts of the heart, in the anterior and posterior walls of the ventricles, in the apex and base of the heart.
Additional leads:
The diagnostic capabilities of an ECG study can be expanded by using some additional leads. Their use is especially advisable in cases where the usual program for recording 12 generally accepted ECG leads does not allow a sufficiently reliable diagnosis of a particular electrocardiographic pathology or requires clarification of some quantitative parameters of the identified changes.The method of registration of additional leads differs in the localization of the active electrode on the surface of the chest.
The active electrode is placed along the posterior axillary (V7), scapular (V8) and paravertebral (V9) lines at the level of the horizontal, on which the electrodes V4-V6 are located. These leads are usually used to more accurately diagnose focal myocardial changes in the posterior basal regions of the left ventricle.
Neb leads. Two-platform chest leads, proposed in 1938 by Neb, fix the potential difference between two points located on the surface of the chest. The Nab leads are recorded at the positions of the switch handle on standard leads, the electrodes of which are placed on the chest: the electrode for the right hand is the II intercostal space at the right edge of the sternum, the electrode for the left hand is at a point located at the level of the apex beat along the left posterior axillary line, for the left leg - to the area of the apical impulse.
Three leads are recorded: D (dorsalis) in the position of the switch on lead I, A (anterior) - on lead II, Y (inferior) - on lead III.
The Nebu leads are used to diagnose focal changes in the myocardium of the posterior wall (lead D), the anterolateral wall (lead A) and the upper sections of the anterior wall (lead Y).
Neb leads are often used when performing bicycle ergometer and other functional electrocardiographic tests with physical activity.
The Lian lead, or S5, is used to clarify the diagnosis of complex arrhythmias; it is recorded when the switch handle is positioned on lead I, the electrode for the right hand is placed in the II intercostal space at the right edge of the sternum, the electrode for the left hand is at the base of the xiphoid process, on the right or left from it, depending on the position of the electrode, the P wave is better detected.
Slapak-Partilla leads are used to clarify changes in the posterior wall in the presence of a deep Q tooth in II, III, AVF leads.
The electrodes are placed as follows: the electrode from the left hand (yellow) is placed along the left posterior axillary line at the level of the apical impulse (V intercostal space), the electrode from the right hand (red) is placed alternately in the II intercostal space at 4 points: 1 - at the left edge of the sternum; 2 - in the middle of the distance between 1 and 3; 3 - on the midclavicular line; 4 - along the anterior axillary line. The ECG is recorded in switching lead I. Receive 4 leads - S1, S2, S3, S4.
When tooth Q grows from S1 to S4, it can be assumed that the patient has cicatricial changes in the posterior wall or acute myocardial infarction (take an ECG over time).
Lead according to Kleten. Clarifies changes in the lower wall of the left ventricle. In this case, the electrode from the right hand is placed on the manubrium of the sternum, the second electrode remains on the left leg. The ECG is recorded in the switch position - standard lead II.
Electrocardiogram recording technique:
To obtain a high-quality ECG recording, you must strictly adhere to some general rules for its registration.Conditions for conducting the study. ECG is recorded in a special room, remote from possible sources of electronic fields: electric motors, physiotherapy and X-ray rooms, electrical distribution panels.
The couch must be located at a distance of at least 1.5-2 m from the electrical wires. It is advisable to shield the couch.
The study is carried out after a 10-15 minute rest, no earlier than 2 hours after eating. The patient must be undressed to the waist, his legs must also be freed from clothing.
An ECG is usually recorded with the patient lying on his back, which allows for maximum muscle relaxation.
Application of electrodes:
4 electrodes (plate electrodes) are placed on the inner surface of the shins and forearms in the lower third, and one or more (for multi-channel recording) chest electrodes are installed on the chest using a rubber suction bulb.To improve recording quality, good contact of the electrodes with the skin should be ensured.
To do this you need:
1) degrease the skin with alcohol in the areas where the electrodes are applied;
2) if the skin is significantly hairy, moisten the areas where the electrodes are applied with a soap solution or shave;
3) place gauze pads moistened with a 5-10% sodium chloride solution under the electrodes, or cover the electrodes with a layer of special conductive paste or gel.
Connecting wires to electrodes:
Each electrode, installed on the limbs or on the chest, is connected to a wire coming from the electrocardiograph and marked with a certain color.Input wire markings:
1) right hand - red;
2) left hand - yellow;
3) left leg - green;
4) right leg (patient grounding) - black;
5) chest electrode - white.
If you have a 6-channel electrocardiograph that allows you to simultaneously record an ECG in 6 chest leads, a wire with a red tip is connected to electrode V1, yellow to electrode V2, green to V3, brown to V4, black to V5, purple to V6.
Recording an electrocardiogram:
In the position of the lead switch “O”, the calibration millivolt is recorded (1 mV = 10 mm).If necessary, you can change the gain: reduce it if the amplitude of the ECG waves is too large (1 mV = 5 mm) or increase it if their amplitude is small (1 mV = 15 or 20 mm).
ECG recording is carried out during quiet breathing. At least 4 cardiac PQRST cycles are recorded in each lead. ECG is recorded, as a rule, at a paper speed of 50 mm/s. A lower speed (25 mm/s) is used when longer ECG recordings are required, for example, to diagnose rhythm disturbances.
The patient's surname, patronymic and first name, his age, date and time of the study are recorded on a paper tape. The ECG tape should be cut into leads and pasted onto the form in the same sequence that was recommended for taking an ECG: I, II, III, AVR, AVL and AVF, V1-V6.
Functional tests:
1) tests with physical activity;2) pharmacological tests are used to distinguish between functional and organic changes in the electrocardiogram.
Test with b-adrenergic receptor blockers:
A test with anaprilin (obzidan) is carried out to clarify the nature of previously identified electrocardiographic disorders of the repolarization process (ST segment and T wave) and to carry out differential diagnosis of functional (neurocirculatory dystonia, dishormonal myocardial dystrophy) and organic (angina pectoris, myocarditis) and other heart diseases.The study is carried out in the morning on an empty stomach. After recording the initial ECG in 12 standard leads, the patient is given 40-80 mg of anaprilin (obzidan) orally and the ECG is recorded again 30, 60 and 90 minutes after taking the drug.
With functional reversible changes in the myocardium, accompanied by changes in the final part of the ventricular complex (ST segments and T wave), taking b-blockers in most cases leads to partial or complete normalization of the ECG (positive test).
Electrocardiographic disorders of an organic nature do not undergo significant changes after taking the drug (negative test).
Under the influence of beta-adrenergic receptor blockers, slight bradycardia and an increase in the duration of the PQ interval are possible. The test is contraindicated in patients with bronchial asthma and heart failure.
Potassium chloride test:
The test is used for the same purpose as the test with b-blockers. After recording the ECG, the patient is given 6-8 g of potassium chloride orally, diluted in a glass of water. The ECG is recorded again 30, 60 and 90 minutes after potassium intake. partial or complete normalization of the previously measured S-T segment and T wave after taking the drug (positive test) occurs, as a rule, with functional changes in the myocardium. A negative test often indicates organic processes in the heart muscle. During the test, nausea and weakness may sometimes occur.An electrocardiographic test with nitroglycerin gives multidirectional changes that are very difficult to interpret. All functional tests are carried out in the morning on an empty stomach or 3 hours after breakfast. The final decision to conduct the test is made on the day of the test, after recording the initial ECG.
Atropine test:
After registration of the ECG, the subject is injected subcutaneously with 1 ml of a 0.1% solution of atropine and the ECG is re-examined after 5, 15 and 30 minutes. The introduction of atropine blocks the action of the vagus nerve and allows a more correct interpretation of the origin of cardiac rhythm and conduction disturbances. For example, if the ECG showed a prolongation of the P-Q interval, and after the administration of atropine, its duration returned to normal, then the existing violation of atrioventricular conduction was due to an increase in the tone of the vagus nerve and is not a consequence of organic damage to the myocardium.Normal electrocardiogram:
Any ECG consists of several teeth, segments and intervals, reflecting the complex process of propagation of an excitation wave through the heart.During the diastole of the heart, action currents do not occur, and the electrocardiograph registers a straight line, which is called the isoelectric. The appearance of action currents is accompanied by the appearance of a characteristic curve.
On the ECG of healthy people, the following elements are distinguished:
1) positive waves P, R and T, negative Q and S; inconsistent positive U wave;
2) intervals P-Q, S-T, T-P and R-R;
3) QRS and QRST complexes.
Each of these elements reflects the time and sequence of excitation of different parts of the myocardium.
Under normal conditions, the cardiac cycle begins with excitation of the atria, which is reflected on the ECG by the appearance of the P wave.
The ascending segment P is due mainly to the excitation of the right atrium, the descending - to the left atrium. The size of this tooth is small, and normally its amplitude does not exceed 1-2.5 mm; duration is 0.08-1.0 s.
Normally, in leads I, II, AVF, V2-V6, the P wave is always positive.
In leads III, AVL, V1, the P wave can be positive, biphasic, and sometimes even negative in leads III and AVL.
In lead AVR, the P wave is always negative.
The P wave is followed by a straight line segment to the Q wave, and if it is not expressed, then to the R wave. This is the P-Q (R) interval. It is measured from the beginning of the P wave to the beginning of the Q wave and corresponds to the time from the beginning of atrial excitation to the beginning of ventricular excitation. The normal duration of the P-Q interval is from 0.12 to 0.20 s and in a healthy person depends mainly on the heart rate: the higher the heart rate, the shorter the P-Q interval.
The ventricular QRST complex reflects the complex process of propagation (QAS complex) and extinction (RS-T segment and T wave) of excitation throughout the ventricular myocardium. The QRS duration, measured from the beginning of the Q wave to the end of the S wave, is 0.06-0.1 s.
If the amplitude of the QRS complex waves is large enough and exceeds 5 mm, they are designated by capital letters of the Latin alphabet Q, R, S, if small (less than 5 mm) - by lowercase letters q, r, s.
The negative wave of the QRS complex immediately preceding the R wave is designated by the letter Q (q), and the negative wave immediately following the R wave is designated by the letter S (s). If only a negative deviation is recorded on the ECG, and the R wave is completely absent, the ventricular complex is designated QS.
The first wave of the complex - the negative Q wave - corresponds to the excitation of the interventricular septum.
Normally, the Q wave can be recorded in all standard and enhanced limb leads and in chest leads V4-V6. The amplitude of the normal Q wave in all leads except AVR does not exceed the height of the R wave, and its duration is 0.03 s.
In the AVR lead in a healthy person, a deep and wide Q wave or even a QS complex may be recorded.
The R wave corresponds to almost complete coverage of both ventricles by excitation. It is the highest tooth of the ventricular complex; its amplitude ranges from 5-15 mm.
Normally, the R wave can be recorded in all standard and enhanced limb leads. In lead AVR, the R wave is often poorly defined or absent altogether. In the chest leads, the R wave amplitude gradually increases from V1 to V4, and then decreases slightly in V5 and V6.
The RV1, V2 wave reflects the spread of excitation along the interventricular septum, and the RV4, V5, V6 wave - along the muscle of the left and right ventricles. The interval of internal deviation in lead V1 does not exceed 0.03 s, and in lead V6 - 0.05 s.
The S wave is recorded when the ventricles are completely covered by excitation.
The amplitude of the S wave varies widely, not exceeding 20 mm. In the chest leads, the S wave gradually decreases from V1, V2 to V4, and in leads V5, V6 it has a small amplitude or is completely absent.
The duration of the ventricular complex is 0.07-0.1 s.
At the moment of complete depolarization of the myocardium, there is no potential difference, therefore, as a rule, a straight line is recorded on the ECG:
1) S-T interval;
2) RS-T segment - a segment from the end of the QRS complex to the beginning of the T wave;
The RS-T segment in a healthy person in the limb leads is located on the isoline (+ 0.5 mm). Normally, in chest leads V1-V3 there may be a slight displacement of the segment (no more than 2 mm), and in leads V4, 5, 6 - downwards (no more than 0.5 mm).
The T wave corresponds to the recovery phase (repolarization) of the ventricular myocardium.
Normally, the T wave is always positive in leads I, II, AVF1, V2-V6, with T1 > TIII, and TV5 > TV1.
In leads III, AVL and V, the T wave can be positive, biphasic or negative.
In AVR leads, the T wave is normally always negative.
The amplitude of the T wave in the limb leads in a healthy person does not exceed 5-6 mm, and in the chest leads - 15-17 mm. The duration of the prong ranges from 0.16 to 0.24 s.
The Q-T interval reflects the time of excitation and recovery of the ventricular myocardium - the electrical system of the ventricles. It varies from the beginning of the Q (or R) wave to the end of the T wave. Its duration depends on the heart rate: as the heart rate increases, the Q-T interval shortens.
In women, the duration of the Q-T interval at the same heart rate is longer than in men.
Electrocardiogram analysis. The analysis should begin with checking the correctness of its registration technique (the presence of interference), the amplitude of the control millivolt, and estimates of the speed of paper movement.
The procedure for deciphering the ECG:
1. Heart rate and conduction analysis includes determining the regularity and number of heartbeats, finding the source of excitation, and assessing the conduction function.Since the normal pacemaker is the sinus node and the excitation of the atria precedes the excitation of the ventricles, the P wave should be located in front of the ventricular complex. The duration of R-R intervals should be the same (+10% of the average R-R duration).
To count the number of heartbeats, you need to set the duration of one cardiac cycle (R-R interval) and calculate how many such cycles are contained in 1 minute.
Heart rate = 60 / R-R.
If the rhythm is incorrect, find the average duration of one R-R interval and then determine the frequency, as with the correct rhythm.
2. The position of the electrical axis of the heart is determined by the shape of the ventricular complexes in standard leads.
The ratio of the size of the R tooth in the normal position of the electrical axis can be represented as R2 > R1 > R3.
The location of the electrical axis changes as the position of the heart in the chest changes. When the diaphragm is low in people of asthenic type, the electrical axis takes a more vertical position, the highest R wave will be recorded in lead III.
When the diaphragm is high in hypersthenics, the electrical axis is located more horizontally, so the highest R wave is recorded in lead I.
3. Changes in the duration and magnitude of individual ECG elements. Measurements are taken in the standard lead where the waves are most pronounced (usually in II).
Wave R. Its amplitude normally does not exceed 2.5 mm, duration -0.1 s. With normal movement of the excitation wave along the atria, the P waves in leads I, II, III are positive, and with the direction of excitation from bottom to top, they are negative.
QRS complex. A pathological Q wave is characterized by an increase in its amplitude to more than 1/4 of the R wave in this lead, and a duration of >0.03 s.
R wave - measure the amplitude, compare with the amplitude of the Q or S wave in the same lead and with the R wave in other leads; measure the duration of the interval of internal deviation in leads V1 and V6.
S wave - measure its amplitude, compare it with the amplitude of the R wave in the same lead.
RS-T segment. Analyzing its condition, it is necessary:
1) find connection point j;
2) measure its deviation from the isoline;
3) measure the amount of displacement of the RS-T segment from the isoline up or down at a point located 0.05-0.08 s from the point to the right;
4) determine the shape of the displacement - horizontal, oblique, oblique, ascending.
T wave - determine the direction (in most leads the T wave is positive), evaluate the shape of the amplitude.
Q-T interval (electrical ventricular systole). The calculation is carried out using the Bezette formula (see above) or using tables.
The clinical significance of electrocardiography cannot be overestimated. It is of great help in identifying heart rhythm disturbances, diagnosing coronary circulatory disorders, hypertrophies of various parts of the heart, and blockades. But with all the value of the method, it is necessary to emphasize that the ECG should be assessed only taking into account clinical and laboratory data, since various pathological processes can lead to similar changes, and the absence of pathological changes is not always the norm (even with myocardial infarction, the patient can die with “normal ” ECG). Ignoring clinical data and overestimating the electrocardiographic method can lead to serious diagnostic errors. The advantage of the method is that it can be used in any conditions and is harmless to the patient. These qualities led to the widespread introduction of electrocardiography into practical medicine.
Electrocardiography I
Electrocardiography
Electrocardiography is a method of electrophysiological study of heart activity in normal and pathological conditions, based on recording and analysis of the electrical activity of the myocardium spreading throughout the heart during the cardiac cycle. Registration is carried out using special devices - electrocardiographs. The recorded curve - () - reflects the dynamics during the cardiac cycle of the potential difference at two points of the electric field of the heart, corresponding to the places on the body of the subject of two electrodes, one of which is the positive pole, the other is negative (connected respectively to the + and - poles of the electrocardiograph). A certain relative position of these electrodes is called an electrocardiographic lead, and a conditional straight line between them is called the axis of this lead. On a normal basis, the magnitude of the electromotive force (EMF) of the heart and its direction, changing during the cardiac cycle, are reflected in the form of the dynamics of the projection of the EMF vector onto the lead axis, i.e. on a line, and not on a plane, as happens when recording a vectorcardiogram (see Vectorcardiography), reflecting the spatial dynamics of the direction of the EMF of the heart in projection onto the plane. Therefore, an ECG, as opposed to a vectorcardiogram, is sometimes called a scalar one. In order to use it to obtain spatial information about changes in electrical processes in, it is necessary to take an ECG at different positions of the electrodes, i.e. in different leads whose axes are not parallel. Theoretical foundations of electrocardiography are based on the laws of electrodynamics applicable to electrical processes occurring in connection with the rhythmic generation of an electrical impulse by the heart pacemaker and the spread of electrical excitation through the conduction system of the heart (Heart) and myocardium. After generating an impulse in the sinus node, it first spreads to the right, and after 0.02 With and to the left atrium, then after a short delay in the atrioventricular node it passes to the septum and synchronously covers the right and left ventricles of the heart, causing them. Each excited one becomes an elementary dipole (two-pole generator): the sum of the elementary dipoles at a given moment of excitation constitutes the so-called equivalent dipole. The spread of excitation throughout the heart is accompanied by the appearance of an electric field in the volumetric conductor (body) surrounding it. The change in the potential difference at 2 points of this field is perceived by the electrocardiograph electrodes and recorded in the form of ECG waves directed upward (positive) or downward (negative) along the isoelectric line, depending on the direction of the EMF between the poles of the electrodes. In this case, the amplitude of the teeth, measured in millivolts or millimeters (usually recording is done in a mode where the standard calibration potential lmv deflects the recorder pen by 10 mm), reflects the magnitude of the potential difference along the axis of the ECG lead. The founder of E., the Dutch physiologist W. Einthoven, proposed recording the potential difference in the frontal plane of the body in three standard leads - as if from the vertices of an equilateral triangle, for which he took the right hand, left hand and pubic (in practical E. as the third vertices the left one is used). The lines between these vertices, i.e. The sides of the triangle are the axes of standard leads. Normal electrocardiogram reflects the process of excitation spreading through the conduction system of the heart ( rice. 3
) and contractile myocardium after generating an impulse in the sinoatrial node, which is normally the pacemaker of the heart. On the ECG ( rice. 4, 5
) during the diastole period (between the T and P teeth), a horizontal straight line is recorded, called the isoelectric (isoline). the impulse in the sinoatrial node propagates along the atrial myocardium, which forms an atrial P wave on the ECG, and simultaneously along the internodal pathways of fast conduction to the atrioventricular node. Due to this, it enters the atrioventricular chamber even before the end of atrial excitation. It goes slowly along the atrioventricular node, therefore, after the P wave to the beginning of the teeth, reflecting the excitation of the ventricles, an isoelectric is recorded on the ECG; During this time, mechanical atrial function is completed. Then the impulse is quickly conducted along the atrioventricular bundle (His bundle), its trunk and legs (branches), the branches of which, through the Purkinje fibers, transmit excitation directly to the fibers of the contractile myocardium of the ventricles. () of the ventricular myocardium is reflected on the ECG by the appearance of Q, R, S waves (QRS complex), and in the early phase - the RST segment (more precisely, the ST or RT segment, if the S wave is absent), almost coinciding with the isoline, and in the main (fast ) phase - the T wave. Often the T wave is followed by a small U wave, the origin of which is associated with repolarization in the His-Purkinje system. First 0.01-0.03 With The QRS complex is due to excitation of the interventricular septum, which is reflected by the Q wave in the standard and left chest leads, and by the beginning of the R wave in the right chest leads. The normal duration of the Q wave is no more than 0.03 With. In the next 0.015-0.07 With the apices of the right and left ventricles are excited from the subendocardial to subepicardial layers, their anterior, posterior and lateral walls, lastly (0.06-0.09 With) excitation spreads to the bases of the right and left ventricles. Integral vector of the heart between 0.04 and 0.07 With complex is oriented to the left - to the positive pole of leads II and V 4, V 5, and in the period 0.08-0.09 With- up and slightly to the right. Therefore, in these leads, the QRS complex is represented by a high R wave with shallow Q and S waves, and in the right chest leads a deep S wave is formed. The ratio of the values of the R and S waves in each of the standard and unipolar leads is determined by the spatial position of the integral vector of the heart of the electrical axis of the heart) , which normally depend on the location of the heart in the chest. Thus, the ECG normally reveals an atrial P wave and QRST, consisting of negative Q, S waves, a positive R wave, as well as a T wave, positive in all leads except VR, in which it is negative, and V 1 -V 2 , where the T wave can be either positive or negative or slightly pronounced. The atrial P wave in lead aVR is also normally always negative, and in lead V 1 it is usually represented by two phases: positive - larger (excitation predominantly of the right atrium), then negative - smaller (excitation of the left atrium). The QRS complex may lack Q and/or S waves (forms RS, QR, R), and also have two R or S waves, with the second wave designated R 1 (forms RSR 1 and RR 1) or S 1 . The time intervals between the same teeth of neighboring cycles are called inter-cycle intervals (for example, P-P, R-R intervals), and between different teeth of the same cycle - intra-cycle intervals (for example, P-Q, O-T intervals). ECG segments between waves are designated as segments if their duration is not described, but in relation to an isoline or configuration (for example, ST, or RT, a segment extending from the end of the QRS complex to the end of the T wave). Under pathological conditions, they can shift upward (elevation) or downward () relative to the isoline (for example, the ST segment upward in myocardial infarction, pericarditis). Sinus rhythm is determined by the presence in leads I, II, aVF, V 6 of a positive P wave, which normally always precedes the QRS complex and is spaced from it (P-Q interval or P-R interval if there is no Q wave) by at least 0 ,12 With. With pathological localization of the atrial pacemaker close to the atrioventricular junction or in it itself, the P wave in these leads is negative, approaches the QRS complex, can coincide with it in time and even be detected after it. The regularity of the rhythm is determined by the equality of intercycle intervals (P-P or R-R). With sinus arrhythmia, the P-P (R-R) intervals differ by 0.10 With and more. The normal duration of atrial excitation, measured by the width of the P wave, is 0.08-0.10 With. The normal P-Q interval is 0.12-0.20 With. The time of propagation of excitation through the ventricles, determined by the width of the QRS complex, is 0.06-0.10 With. Duration of electrical systole of the ventricles, i.e. The Q-T interval, measured from the beginning of the QRS complex to the end of the T wave, normally has the proper value depending on the heart rate (proper Q-T duration), i.e. on the duration of the cardiac cycle (C), corresponding to the R-R interval. According to Bazett's formula, the proper Q-T duration is equal to k, where k is a coefficient of 0.37 for men and 0.39 for women and children. An increase or decrease in the Q-T interval by more than 10% compared to the expected value is a sign of pathology. The amplitude (voltage) of normal ECG waves in different leads depends on the physique of the subject, the severity of the subcutaneous tissue, and the position of the heart in the chest. In adults, the normal P wave is usually the highest (up to 2-2.5 mm) in lead II; it has a semi-oval shape. PIII and PaVL - positive low (rarely shallow negative). with a normal location of the electrical axis of the heart, it is presented in leads I, II, III, aVL, aVF, V 4 -V 6 shallow (less than 3 mm) an initial Q wave, a high R wave and a small final S wave. The highest R wave in leads II, V 4, V 5, and in lead V 4 the amplitude of the R wave is usually greater than in lead V 6, but does not exceed 25 mm (2,5 mV). In lead aVR, the main wave of the QRS complex (S wave) and the T wave are negative. In lead V, the rS complex is recorded (lowercase letters denote teeth of relatively small amplitude, when it is necessary to specifically emphasize the ratio of amplitudes), in leads V 2 and V 3 - the RS or rS complex. The R wave in the chest leads increases from right to left (from V, to V 4 -V 5) and then decreases slightly to V 6 . The S wave decreases from right to left (from V 2 to V 6). The equality of the R and S waves in one lead determines the transition zone - the lead in the plane perpendicular to the spatial vector of the QRS complex. Normally, the transition zone of the complex is located between leads V 2 and V 4. The direction of the T wave usually coincides with the direction of the largest wave of the QRS complex. It is positive, as a rule, in leads I, II, Ill, aVL, aVF, V 2 -V 6 and has a greater amplitude in those leads where the R wave is higher; and the T wave is 2-4 times smaller (with the exception of leads V 2 -V 3, where the T wave can be equal to or higher than R). The ST segment (RT) in all limb leads and in the left chest leads is recorded at the level of the isoelectric line. Small horizontal displacements (down to 0.5 mm or up to 1 mm) of the ST segment are possible in healthy people, especially against the background of tachycardia or bradycardia, but in all such cases it is necessary to exclude the nature of such shifts by dynamic observation, functional tests or comparison with clinical data. In leads V 1, V 2, V 3, the RST segment is located on the isoelectric line or is shifted upward by 1-2 mm. Variants of a normal ECG, depending on the location of the heart in the chest, are determined by the ratio of the R and S waves or the shape of the QRS complex in different leads; in the same way, pathological deviations of the electrical axis of the heart are identified with hypertrophy of the ventricles of the heart, blockade of the branches of the His bundle, etc. These options are considered conventionally as rotations of the heart around three axes: anteroposterior (the position of the electrical axis of the heart is defined as normal, horizontal, vertical, or as its deviation to the left, right), longitudinal (rotation clockwise and counterclockwise) and transverse (rotation of the heart by the apex forward or backward). The position of the electrical axis is determined by the value of the angle α, constructed in the coordinate system and axes of abduction from the limbs (see. rice. 1, a and b
) and calculated from the algebraic sum of the amplitudes of the QRS complex teeth in each of any two limb leads (usually I and III): normal position - α from + 30 to 60°: horizontal - α from 0 to +29°; vertical α from +70 to +90°. deviation to the left - α from -1 to -90°; to the right - α from +91 to ±80°. When the electrical axis of the heart is horizontal, the integral vector is parallel to the T axis of the lead; the R I wave is high (higher than the R II wave); R III SVF. When the electrical axis deviates to the left, R I > R II > R aVF When the heart rotates around the longitudinal axis clockwise, the ECG shows an RS shape in leads I, V 5.6 and a qR shape in lead III. When rotated counterclockwise, the ventricular complex has a qR shape in leads I, V 5.6 and an RS shape in lead III and a moderately increased R in leads V 1 -V 2 without displacement of the transition zone (in lead V 2 R In children, a normal ECG has a number of features, the main of which are: deviation of the electrical axis of the heart to the right (α is +90 - +180° in newborns, +40° - +100° in children aged 2-7 years); the presence in leads II, Ill, aVF of a deep Q wave, the amplitude of which decreases with age and becomes close to that in adults by 10-12 years; low voltage of the T wave in all leads and the presence of a negative T wave in leads III, V 1 -V 2 (sometimes V 3 , V 4), shorter duration of P waves and QRS complex - an average of 0.05 With in newborns and 0.07 With in children from 2 to 7 years old; shorter P-Q interval (average 0.11 With in newborns and 0.13 With in children from 2 to 7 years old). By the age of 15, the listed ECG features are largely lost, the duration of the P wave and the QRS complex averages 0.08 each With, P-Q interval - 11.14 With. Electrocardiographic changes in the state and activity of the heart is based on an analysis of the size, shape, direction in different leads and repeatability in each cycle of all ECG waves, measurement data of the duration of the P, Q waves, the QRS complex and the P-Q (P-R), Q-T intervals, R-R, as well as deviations from the isoline of the RST segment with subsequent interpretation of the identified features as pathological or as a variant of the norm. The protocol part of the ECG report must characterize the heart rhythm (sinus, ectopic, etc.) and the position of the electrical axis of the heart. The conclusion contains characteristics of a specific pathological ECG syndrome. In a number of forms of heart pathology, the totality of ECG changes has a certain specificity, and therefore E. is one of the leading diagnostic methods in cardiology. Dextrocardia due to a mirror change in the topography of the heart relative to the sagittal plane and its displacement to the right, it determines the orientation of the main vectors of excitation of the atria and ventricles of the heart to the right, i.e. to the negative pole of lead I and to the positive pole of lead III. Therefore, on the ECG in lead I, a deep S wave and negative P and T waves are recorded; the R III wave is high, the P III and T III waves are positive; in the chest leads, the QRS voltage is reduced in the left positions with an increase in the depth of the S wave towards leads V 5 -V 6 .
If you swap the electrodes of the right and left hands, then the ECG shows waves of the usual shape and direction in leads I and III. Such replacement of electrodes and registration of additional chest leads V 3R, V 4R, V 5R, V 6R make it possible to confirm the conclusion and identify or exclude other myocardial pathology in dextrocardia. With dextroversion, unlike dextrocardia, the P wave in leads I, II, V 6 is positive. the initial part of the ventricular complex has a qRS shape in leads I and V 6 and an RS shape in lead V 3R. Hypertrophy of the atria and ventricles of the heart is accompanied by an increase in the EMF of the hypertrophied section and a deviation in its direction of the vector of the total EMF of the heart. On the ECG, this is reflected in certain leads by an increase and (or) change in the shape of the P waves with atrial hypertrophy and the R and S waves with ventricular hypertrophy. There may be a slight widening of the corresponding tooth and an increase in the so-called internal deviation, i.e. time from the beginning of the P wave or ventricular complex to the moment corresponding to the maximum of their positive deflection (the top of the P or R wave). With ventricular hypertrophy, the final part of the ventricular complex may change: the RST moves downward and becomes lower or the T wave in leads with high R is inverted (becomes negative), which is designated as (multidirectional) ST segment and T wave in relation to the R wave. A segment is also observed RST and T wave relative to the S wave in leads with a deep S wave. With left atrial hypertrophy ( rice. 7
) the P wave expands to 0.11-0.14 With, becomes double-humped (P mitrale) in leads I, II, aVL and left thoracic, often with an increase in the amplitude of the second apex (in some cases the P wave is flattened). Time of internal deviation of the P wave in leads I, II, V 6 more than 0.06 With. The most common and reliable sign of left atrial hypertrophy is an increase in the negative phase of the P wave in lead V1, which becomes larger in amplitude than the positive phase. Right atrial hypertrophy ( rice. 8
) is characterized by an increase in the amplitude of the P wave (more than 1.8-2.5 mm) in leads II, Ill, aVF, its pointed form (P pulmonale). The electrical axis of the P wave acquires a vertical position, less often deviated to the right. A significant increase in the amplitude of the P wave in leads V 1 -V 3 is observed with congenital heart defects (P congenitale).